Ketamine clinics are increasing in number in the United States and globally. As we described previously, ketamine is a Schedule III drug under the federal Controlled Substances Act, has been approved by the Food and Drug Administration (FDA) for certain medical uses, and may in some cases be used for off-label uses (such as anxiety or depression) by medical professionals. That said, the legal framework surrounding the ownership and operation of ketamine clinics (which involve off-label uses of ketamine) can be extraordinarily complicated and will vary significantly from jurisdiction to jurisdiction.
California is certainly a place where ketamine clinics are prominent. The corporate structures of many ketamine clinics involve a risky dance when it comes to the corporate practice of medicine. Ownership of medical practice in California is highly regulated. There are significant restrictions on who can own a medical practice here; that includes ketamine infusion clinics because only licensed medical practitioners can prescribe and manage ketamine and corresponding treatments.
California law requires that a medical practice be owned by a specific entity (a professional medical corporation) and that a majority of owners of the corporation be physicians with limits on ownership by non-physicians to other medical professionals. There are similar laws for medical partnerships. What this means is that ketamine clinics must generally be owned by licensed physicians, and cannot have owners who are not licensed medical professionals. That said, there is still a narrow possibility for non-medical professional business ventures with ketamine clinics: namely though the management-services organization (MSO) model.
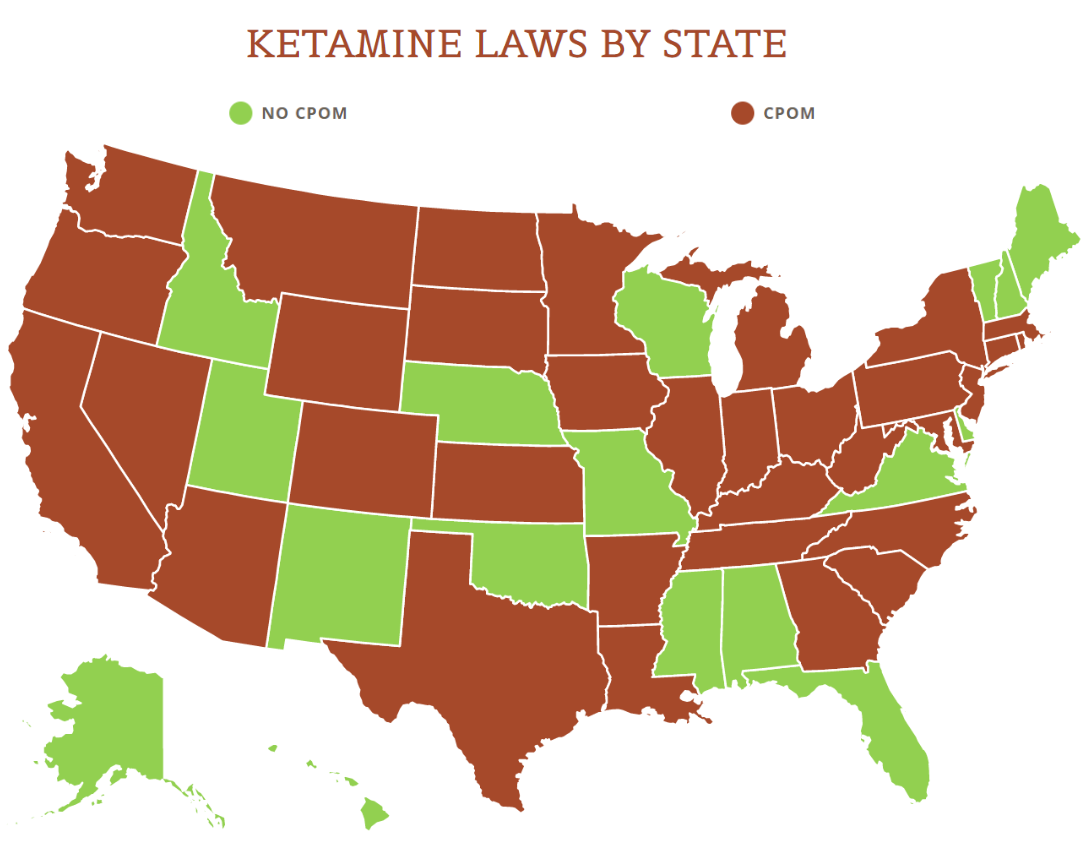
View the US Map of Ketamine Legality
MSOs may at first sound a lot like the typical management company, but they are very different and they’re very limited in what they can do. The California Medical Board states that physicians cannot delegate the following to MSOs or non-physicians:
- Ownership is an indicator of control of a patient’s medical records, including determining the contents thereof, and should be retained by a California-licensed physician.
- Selection, hiring/firing (as it relates to clinical competency or proficiency) of physicians, allied health staff and medical assistants.
- Setting the parameters under which the physician will enter into contractual relationships with third-party payers.
- Decisions regarding coding and billing procedures for patient care services.
- Approving of the selection of medical equipment and medical supplies for the medical practice.
The Medical Board also prohibits the following conduct:
- Non-physicians owning or operating a business that offers patient evaluation, diagnosis, care and/or treatment.
- Physician(s) operating a medical practice as a limited liability company, a limited liability partnership, or a general corporation.
- Management service organizations arranging for, advertising, or providing medical services rather than only providing administrative staff and services for a physician’s medical practice (non-physician exercising controls over a physician’s medical practice, even where physicians own and operate the business).
- A physician acting as “medical director” when the physician does not own the practice. For example, a business offering spa treatments that include medical procedures such as Botox injections, laser hair removal, and medical microdermabrasion, that contracts with or hires a physician as its “medical director.”
How MSOs can be paid is also extremely complex. Physicians are prohibited by California law for paying for referrals, but the following may be permitted:
The payment or receipt of consideration for services other than the referral of patients which is based on a percentage of gross revenue or similar type of contractual arrangement shall not be unlawful if the consideration is commensurate with the value of the services furnished or with the fair rental value of any premises or equipment leased or provided by the recipient to the payer.
In other words, it is possible that fee-splitting arrangements with MSOs could be legally justified in come cases, but it’s not a given and the law here is very complicated.
This explanation really just scratches the surface of the many issues surrounding the structure of ketamine clinics. The bottom line for ketamine clinics is that ownership and operational issues are not at all straightforward, especially in the context of the general prohibition in California on the corporate practice of medicine. And to make matters more difficult, ketamine clinics are subject to a whole host of other state and federal requirements on physicians and healthcare providers. Tread carefully and look for competent counsel if you plan to enter this trending space.