In recent years, the United States has seen a proliferation of ketamine clinics. From 2015 to 2018, the number of clinics increased from 60 to 300; that number is undoubtedly higher today. People are increasingly using ketamine for ailments that resist treatment through traditional pharmaceutical drugs.
In an even larger trend, the health care provider community seems to be exploring various alternative therapies and emerging medicines to improve quality of care. Recently, the decriminalization of psilocybin (by various cities) has been in the news as an emerging medicine. Similar to ketamine, psilocybin has shown great promise in clinical trials for helping to effectively treat depression and PTSD (and we’ve written about psilocybin several times on this blog, including here and here).
With respect to ketamine infusion therapy (which is the prime time attraction of ketamine clinics), the medical research based promise is for treatment of chronic neuropathic pain, chronic pain (instead of opioids), and various medication-resistant mental health disorders, including depression, bi-polar disorder, and PTSD (among others). According to the American Psychiatric Nurses Association:
Ketamine infusion therapy involves the administration of a single infusion or a series of infusions for the management of psychiatric disorders (e.g., major depressive disorder, post-traumatic stress disorder, acute suicidality). Ketamine is a noncompetitive N-methyl-D-aspartate (NMDA) receptor antagonist that has traditionally been used for the induction and maintenance of anesthesia.
Still, for all its promise, would-be clinic owners, practitioners, and consumers may be confused about the legality of such clinics. There are questions about the logistics of opening and running one of these types of businesses, given the complex interplay of laws and regulations promulgated by bodies from the U.S. Food and Drug Administration (FDA) to cities and counties. This post is dedicated to clearing up some of the confusion behind ketamine clinic set-up and operation.
Is Ketamine Legal in the U.S.?
Ketamine is legal for medicinal use in many countries worldwide— including the U.S. — and some derivatives have also achieved governmental approval.
Yet, usage is regulated, so only licensed and ketamine-experienced practitioners can prescribe it or oversee its administration. This restriction ensures proper delivery and dosage for treatment effectiveness and benefits.
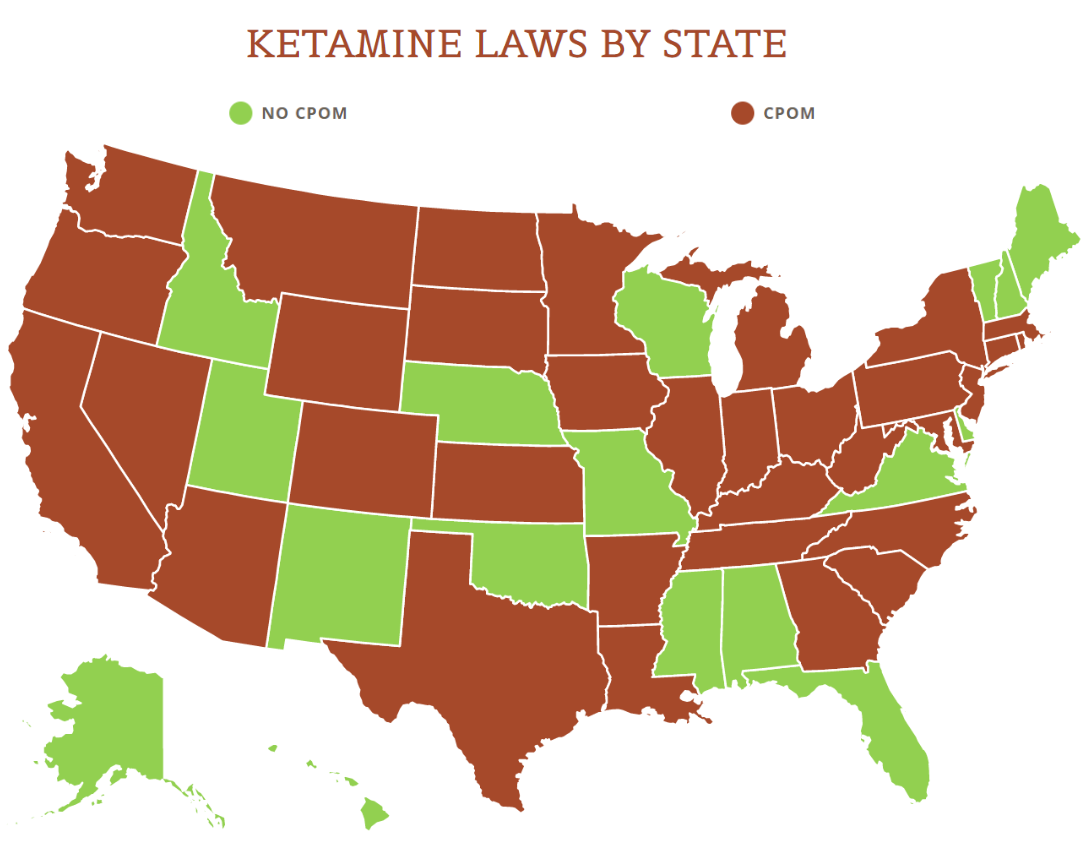
View the US Map of Ketamine Legality
When is it Illegal to use Ketamine?
Despite its popularity as a recreational drug, ketamine remains illegal to use without a prescription or during a surgical procedure under the care of a licensed professional. Clinicians can help manage any side effects the drug could produce. These effects may include symptoms like nausea, dizziness, faster heart rates and higher blood pressure.
Another potential side effect of recreational use without medical supervision is severe dissociation. In simple terms, this means a feeling of disconnection, surrealism or memory gaps. Recreational users refer to this as a “k-hole.”
What are the Exact Legalities Behind Ketamine?
When examining the legal standing of ketamine as a therapeutic, it’s important to differentiate between the federal government’s perspectives and that of individual states.
The federal stance
Sine 1970, ketamine has only been approved by the FDA for the induction and maintenance of anesthesia. However, it is also being used for off-label infusions for the management of psychiatric disorders and chronic pain management (enter the clinics). The FDA doesn’t have any regulations on point for the control and oversight of ketamine clinics when it comes to infusion therapy and the states don’t really either.
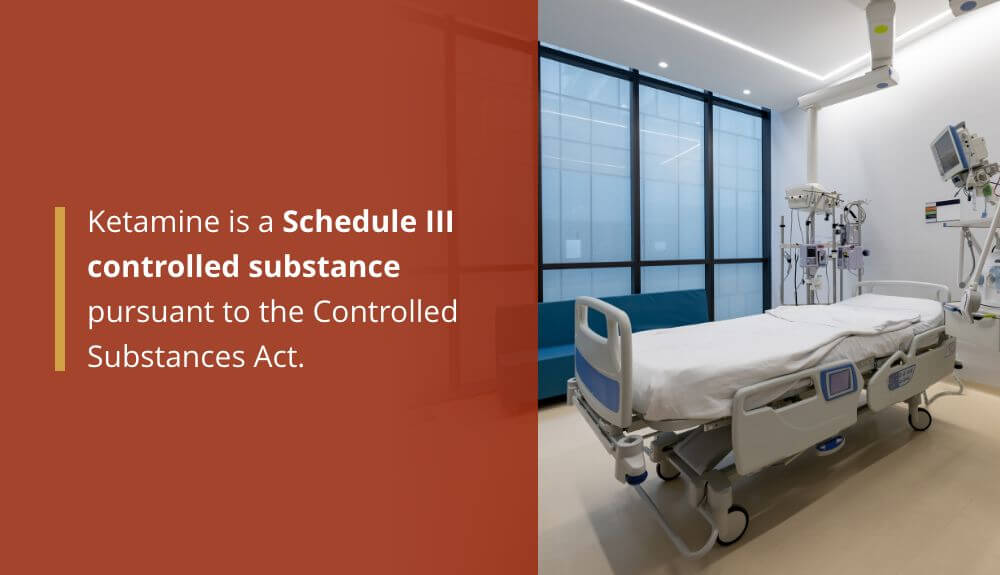
In 1999, the Drug Enforcement Administration (DEA) listed ketamine as a Schedule III controlled substance (a depressant) pursuant to the Controlled Substances Act, which means it has a moderate to low abuse potential (lower than Schedules I and II), a currently accepted medical use, and a low to moderate potential for physical or psychological dependence. Ketamine makes its home on Schedule III alongside anabolic steroids and testosterone. According to the Feds, ketamine is safer than cannabis (which is a Schedule I controlled substance).
So, how does one lawfully open and operate a ketamine clinic for infusion therapy given the foregoing?
First, ketamine infusion therapy is an off-label use for ketamine in the U.S. “Off-label use” (which is extremely common) is:
the use of pharmaceutical drugs for an unapproved indication or in an unapproved age group, dosage, or route of administration. Both prescription drugs and over-the-counter drugs (OTCs) can be used in off-label ways, although most studies of off-label use focus on prescription drugs.
According to the FDA, “once the FDA approves a drug, healthcare providers generally may prescribe the drug for an unapproved use when they judge that it is medically appropriate for their patient.” Oftentimes, a healthcare provider may prescribe a drug off-label because there might not be an approved drug out there yet to treat the subject medical condition or because no other medication has worked yet for the patient.
Ketamine infusion therapy fits squarely into legitimate off-label use for those mental health conditions not effectively treated by what’s on the pharmaceutical market today (and there are definitely more treatment possibilities out there as medical research continues). And as long as the healthcare provider in charge judges the infusion therapy to be ethical and not violative of safety standards, they may prescribe it accordingly.
General State Perspective
Most states mirror the federal acceptance of off-label usage and permit ketamine treatment in clinical settings under the supervision of a medical professional. Some have also begun to issue specific guidelines for ketamine use as a viable medical therapy. The definition of a medical professional, the scope of their duties, and the licensing and permit requirements vary widely from state to state.
Arizona
Ketamine legality in AZ excludes registered nurses other than certified registered nurse anesthetists (CRNAs) from sole administration for anesthetic purposes. They may treat patients for sedation, depression or analgesia — pain relief — under certain circumstances. To do so, all of the following must be true:
- The treatment is a sedation-level dose given by IV or nasal therapy and prescribed by a licensed practitioner.
- A clinician is on-site throughout the process to manage potential effects.
- The pharmacy must prepare the IV solution.
- The nurse completed documented classroom learning and supervised clinical-based training on ketamine.
- The facility has measures in place to monitor patients, deliver the correct dosage and handle any complications.
- Nurses monitor vital signs, including blood oxygen, pulse, blood pressure and sedation level, using a recognized scale.
Ketamine laws in Arizona require analgesic use records to have documentation of additional information, including the treatment duration, dosage, indications and contraindications, and any adverse reactions or side effects.
California
Under current ketamine laws in California, it is a violation of state law to possess ketamine without a prescription or to have more than the recommended quantity allowed by prescription. Unapproved possession can merit a misdemeanor charge. Yet, the state also recognizes that personal possession correlates with personal use and can recommend a drug treatment program that nullifies possession charges against you.
Regardless of the legal status of ketamine in California, it is illegal to operate a motor vehicle when under the drug’s influence.
Ketamine sale or possession with the intent to sell carries steep penalties and no possibility of a treatment program charge dismissal. Depending on the possession quantity, other facts and your criminal history, the state can pursue a misdemeanor or a felony. Fines and prison time vary based on the specific points in the case.
Florida
Florida’s ketamine legal status is complex, particularly surrounding treatment delivery for depression. As the drug remains unapproved for many mental health disorders at the federal level, ketamine laws in Florida are strict regarding both personal possession and treatment by mental health professionals.
The state has a zero-tolerance policy for personal possession, though legal defenses exist and can result in the dismissal of charges. Florida’s perspective on DEA drug schedules is that the highest-tier drugs — those on Schedule I — deserve higher penalties. With ketamine ranking right in the middle at Schedule III, interpretation is more uncertain about how aggressive a prosecutor may be. Factors affecting penalties can range from criminal history to quantity and intent.
Florida considers administering the drug a practice of medicine and has very rigid standards regarding ownership, licensing and pharmaceutical permits. Mental health professionals must understand the state licensing requirements for owning and operating a clinic where ketamine therapy may be an option.
New York
Ketamine laws in New York are generally straightforward. The state permits off-label use in clinical settings but seeks aggressive prosecution for those possessing controlled substances without a prescription.
For medicinal use, it allows legal ketamine treatment in a medical facility under the supervision of a licensed physician. Several university hospital-based clinics regularly offer IV ketamine treatments as a viable therapy for depression despite the lack of FDA approval for the indication.
Possession of ketamine outside the clinical setting can produce a misdemeanor or felony. Generally speaking, small amounts of any drug other than marijuana for personal use constitute a misdemeanor. Having more than 1,000 milligrams of ketamine in your possession without a prescription is a fifth-degree felony.
Oregon
Ketamine laws in Oregon differ from those found elsewhere. The state’s voters supported the reclassification of small amounts of all drugs from Class A misdemeanors to simple violations, provided they are for personal use. That means a $100 fine and completing a mental health assessment by a licensed professional.
Oregon ketamine treatment laws allow certified nurse anesthetists to administer intranasal and IV ketamine therapy in clinical settings as long as a licensed physician prescribes the drug. Other restrictions — such as procedures for managing complications — may also apply.
Utah
Ketamine is legal in Utah according to the off-label use allowed by the FDA. As in other states, treatment delivery must occur in a clinic under the supervision of licensed medical professionals. Practitioners must also abide by different state laws regarding medical practice, patient monitoring and complication management.
Possession of ketamine laws in Utah classify infractions as a class B misdemeanor unless the individual had an intent to sell. Punishments vary and may be affected by other circumstances, including where the individual possessed or used the drug and the presence of prior convictions for similar offenses.
Washington
Washington’s status on ketamine legality is in line with many other states, where off-label use occurs regularly as prescribed by physicians and takes place in a properly licensed clinic.
For ketamine possession outside of facility use, one must have a prescription and not exceed the prescribed quantity. If the court finds you in violation of those circumstances, you may receive a misdemeanor charge. The state also encourages prosecutors to refer someone charged with personal possession to drug treatment programs instead of pursuing a conviction
How Does One Lawfully Open and Operate a Ketamine Clinic for Infusion Therapy Given the Foregoing?
Second, ketamine is still a controlled substance even if it’s being used for off-label administration, so you still have to follow all federal and state laws around Schedule III registration, storage, inventory management, security, record keeping, and prescription protocols (which is not insignificant). Whomever on site is administering, manufacturing, storing, or distributing the drug, from the doctor to the nurse practitioner to the on-site pharmacist, must register with the DEA in accordance with Part 1301 of Title 21 of the Code of Federal Regulations on and after August 12, 1999. Failure to follow these very specific legal directives can lead to immediate criminal liability under federal law.
Third, multiple existing federal and state laws and regulations will apply to a ketamine clinic. Specifically, clinics should analyze state (and federal) medical, drug and facility statutes and regulations to identify various regulatory barriers to entry. Local laws will also likely come into play regarding the licensing and permitting of the clinic within certain zones of a city’s or county’s borders.
Fourth, because there is no FDA regulation on point for the control and oversight of ketamine clinics, it’s “dealer’s choice” on how the business is operated– including patient safety protocols. Because of this, multiple medical community interest groups have established recommended business and patient protocols to ensure that these clinics are abiding by a variety of ethical and corporate standards for ultimate patient care. See, for example, this comprehensive ketamine infusion therapy checklist developed by the American Association of Nurse Anesthetists.
Fifth, given that ketamine infusion therapy is still an off-label use, the liabilities for ketamine clinics is fairly far-reaching. The consequences of medical malpractice may be greater because of the off-label use of the drug; dosing and frequency of treatments, marketing and promotions, medical claims and statements of efficacy, patient screening and determination of appropriateness of administration, and coordination with mental health care providers (to name just a few) are going to be areas of vulnerability as a result.
Despite the growing body of research behind ketamine as an effective treatment for certain mental health issues and mood disorders, in 2017, an American Psychiatric Association (APA) task force related to ketamine cautioned medical practitioners (in a consensus statement) around the expanding use of the drug as an off-label treatment.
Ketamine is also widely known as a popular party drug (“Special K“). If a clinic is not scrupulous regarding its patient population and intake procedures (using minimal screening and untrained providers), or is looking to make a buck over a growing medical fad, anyone could get access to ketamine infusions. That access would be available under the auspices of having a chronic, untreatable mood disorder. As such, legitimate concerns also exist that legitimate patients won’t get enough of the treatment or they’ll get too much of the drug to their detriment.
Finally, esketamine nasal spray (a derivative of ketamine) was separately approved by the FDA for treatment-resistant depression last year. The new drug’s name is Spravato and its maker is Janssen, a division of Johnson & Johnson. On the back of this FDA approval, I can only imagine that more and more clinics will open across the nation, utilizing Spravato and continuing to explore off-label uses and applications of ketamine (especially since neither the FDA or DEA have really cracked down on these clinics).
Be sure to stay tuned as this exciting area of emerging medicine evolves.